Warning: This story contains graphic details about suicide and suicidal ideation.
Nikki says she first had the urge to cut herself at the age of 10, when her grandfather passed away. Shortly after having suicidal thoughts, she started self-harming.
“It helped me escape reality,” the 19 year-old youth from East York told the Toronto Observer. “It helped me inflict pain on myself because I just wanted to feel the pain; I also wanted the pain to go away, too.”
She has had multiple suicide attempts.
“I have been battling depression, anxiety, PTSD, and child-development trauma for the longest time,” she said. (For privacy reasons, we are using Nikki’s first name only, and she is not the person pictured in the top photo of this story.)
Besides having a difficult upbringing, Nikki said she was also sexually assaulted, which led to her last suicide attempt in 2020.
But, she is still here.
She stopped self harming when she found out she was pregnant a few months after her last suicide attempt. She saw the positive result of the pregnancy test, and made up her mind.
“My son helped me, he didn’t stop me from drowning, but he showed me how to swim,” Nikki said.
In Canada, suicide is the second-leading cause of death among youth and young adults aged 15-34 years-old, according to Public Health Canada. The leading cause of death is unintentional injuries.
Youth are also at a higher risk of developing mental illness and substance-use disorders than any other age group. And according to the Centre for Addiction and Mental Health (CAMH), First Nations youth, die by suicide six times more often than non-Indigenous youth.
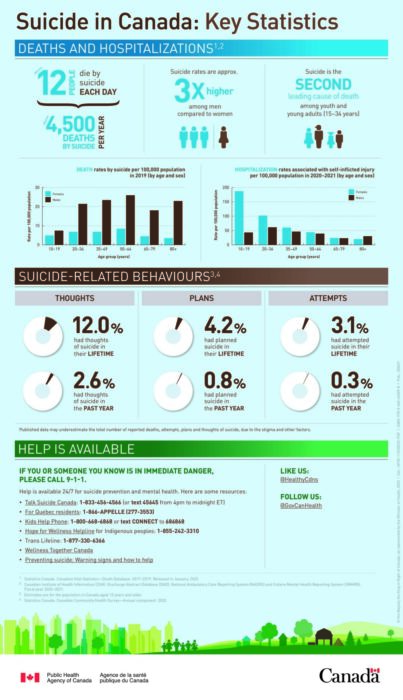
Infographic from Public Health Canada with statistics about suicide in Canada. (Public Health Canada).
According to the Canadian Institute for Health Information, 58 per cent of females aged 15 to 17 are two times more likely to be hospitalized due to a mental health disorder then males of the same age group.
Dr. Toula Kourgiantakis, Assistant Professor, Teaching Stream Factor-Inwentash Faculty of Social Work at the University of Toronto, is a social worker and family therapist.
She said although there are some resources out there for mental-health issues in youth, there are not a lot of resources available.
Mental-health care system ‘not very welcoming’: expert
She also said it is very difficult for young people to have to try to navigate the mental health-care system; it is too complex for a youth in distress.
“It’s difficult for somebody who’s not in distress to try to navigate our very complicated mental-health care system that is actually not very welcoming,” she said.
Kourgiantakis said long wait lists and complicated procedures to access services are barriers to youth clients who need them. And some services are not culturally responsive.
“It just makes it very difficult that we are expecting a youth who is in distress to find the right service, to land on the right person, to sound motivated, to follow up two months later to find out what’s going on with [their] referral,” Kourgiantakis said. “Is it still on the waitlist, or even just to wait on a waitlist?”
Early intervention critical
Kourgiantakis said it’s important to address mental-health issues as soon as possible.
“There is ample research on the importance of early intervention; [it] means we intervene, as soon as symptoms start to present,” she said. “We don’t wait until the symptoms escalate, and the person is in a worse state than they were if we had offered services right from day one.”
Nikki said that in our society there is a lack of understanding with the importance of suicide.
“People fail to understand the importance of suicide because they take it as attention seeking, when in reality, it is not attention seeking,” she said. “Suicidal youth need serious help. And their parents, not only their parents, people around them, their community is failing them,” Nikki said.
Nikki is currently receiving help for her mental-health from a mental-health care home, SickKids, victim services, and a few more organizations. Nikki said she is grateful for all the resources that her social worker connected her with.
‘No call to the family’
Kourgiantakis said that mental health services need to be reorganized; families are also not often welcomed into their youths’ care and are not given enough resources to support them.
Through the pandemic, Kourgiantakis had a client describe their experience of being in crisis in the waiting room at a hospital, where they were sitting alone, for five hours.
The youth was discharged from the hospital because they were not viewed to be in imminent risk, Kourgiantakis said.
“No call to the family … basically the youth was on the street and was suicidal,” she said. This is just one of many examples that she has heard about.
Kourgiantakis said there was also a need for more continuity between services, and that there is not currently enough integration of mental health and addiction services. She also said the system does not have a culturally responsive approach.
“It’s really about having services that are more culturally responsive, and that are not oppressive, that are not discriminatory, that are not stigmatizing, that are equitable and give opportunities for all youth to access them to get the type of quality care that they deserve.”
Dr. Toula Kourgiantakis, professor, social worker and therapist
“It’s quite often that families that are worried sick that might not know how to respond,” Kourgiantakis said.”Which is actually even more reason why they need to be involved, because it would help to equip them on how to respond more supportively.”
She said that mental-health services need to get back to in-person delivery. Video or audio calls might be accessible for some youth that don’t have transportation due to living in rural communities or in situations where they can’t get a service, but for many youth, it is not the ideal modality, she said.
“I think that clinicians, service providers need to always think about the client,” she said. “Is a service benefiting the client to do it virtually? Or is the service benefiting the clinician who wants to work from home?”
She says that there needs to be oversight on how the mental-health services are being organized, especially in public institutions because tax payer dollars are paying for the services.
“It’s really about having services that are more culturally responsive, and that are not oppressive, that are not discriminatory, that are not stigmatizing, that are equitable and give opportunities for all youth to access them to get the type of quality care that they deserve.” Kourgiantakis said.
Factors that affect mental-health in youth
According to one expert, there are multiple issues that youth with mental health face, and one major one is employment.
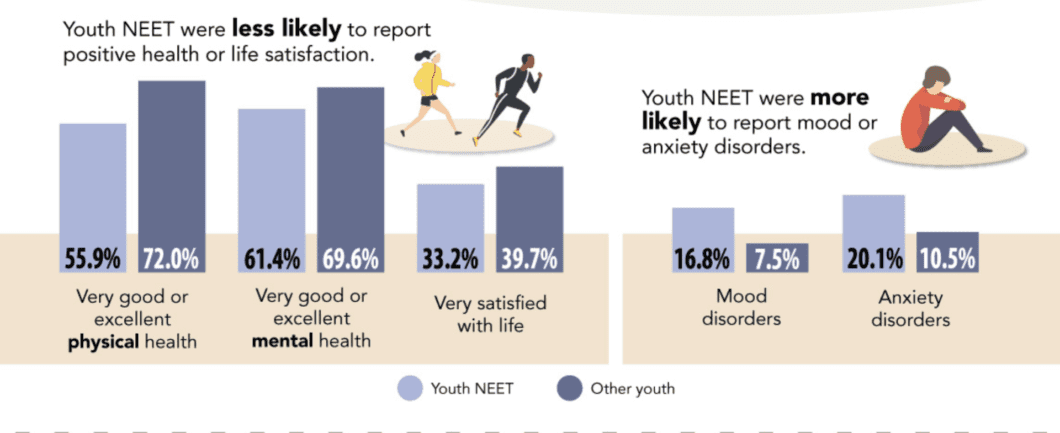
This image shows that youth unemployed, not in school, or training, are more likely to have mental health issues. This infographic is displaying statistics from 2015-2017. (2020/StatisticsCanada)
“Employment gives people a sense of community, a sense of belonging, a sense of self worth, and of course an income,” Timothy Lang, President and CEO of YES employment services (Youth Employment Services), said.
“That’s why organizations like ours at YES, when we bring people together and have that human interaction and have that positive voice, it definitely helps.”
YES is a Canadian youth employment services program that has over 25 youth employment programs, with mental health programs as well. They help approximately 15,000 youth annually. They also claim to have close to a 90 per cent success rate in getting youth employed.
“Of our 25 programs, we have specialized mental health programs for any youth that is diagnosed with any mental health issue, it’s called our YES Lighthouse program and it’s the best in the country.”
Lang said their mental-health programs are designed to help create resilience and help build life skills.
“We work closely with CAMH, which is the clinical leader, but YES is the Canadian leader for employment purposes, and we work with youth with mental health, and do a number of the same things, but we add other mental health aspects to it like cognitive behavioural therapy and other areas that really help the self-esteem and then we place them into employment,” he said.
Lang said organizations, schools, universities, and colleges should educate themselves on how to be better at understanding and adapting to youth with mental-health illnesses.
YES educates companies across the country about mental health and how it can positively impact their business as well as the person that they help and hire.
“We also work with businesses across the country to help businesses understand that there shouldn’t be a stigma against mental health because sometimes with just a small accommodation, you can change not only someone’s life, but they become very long-term loyal employees and a good employee.”
If you or someone you know is struggling with their mental health, help is available.
YES is a free employment service provider and to contact them you can visit their website https://www.yes.on.ca/, or call 416-504-5516
You can speak to someone through different helplines:
1-833-456-4566 – (Talk Suicide Canada)
1-888-668-6810 or text WELLNESS to 686868 – (Wellness Together Canada)
1-800-668-6868 (toll-free) or text CONNECT to 686868 – (Kids Help Phone)
1-866-925-5454 – (Good2Talk)
If this is a life threatening situation, or you or someone you know is in immediate danger, please call 911, or go to the nearest hospital or emergency department.